Emergency cancer – detailed information
Why Emergency Cancer? (“Blåljuscancer” in Swedish)
- Has 5 of the 6 worst predictions for 5-year survival rate
- No obvious symptoms which usually means late detection
- Only few good treatment methods
- Few ongoing studies in our types of cancer
- Lifelong treatment with severe side effects often required
MENU Emergency cancer
Emergency cancer overall
Emergency cancer – detailed info
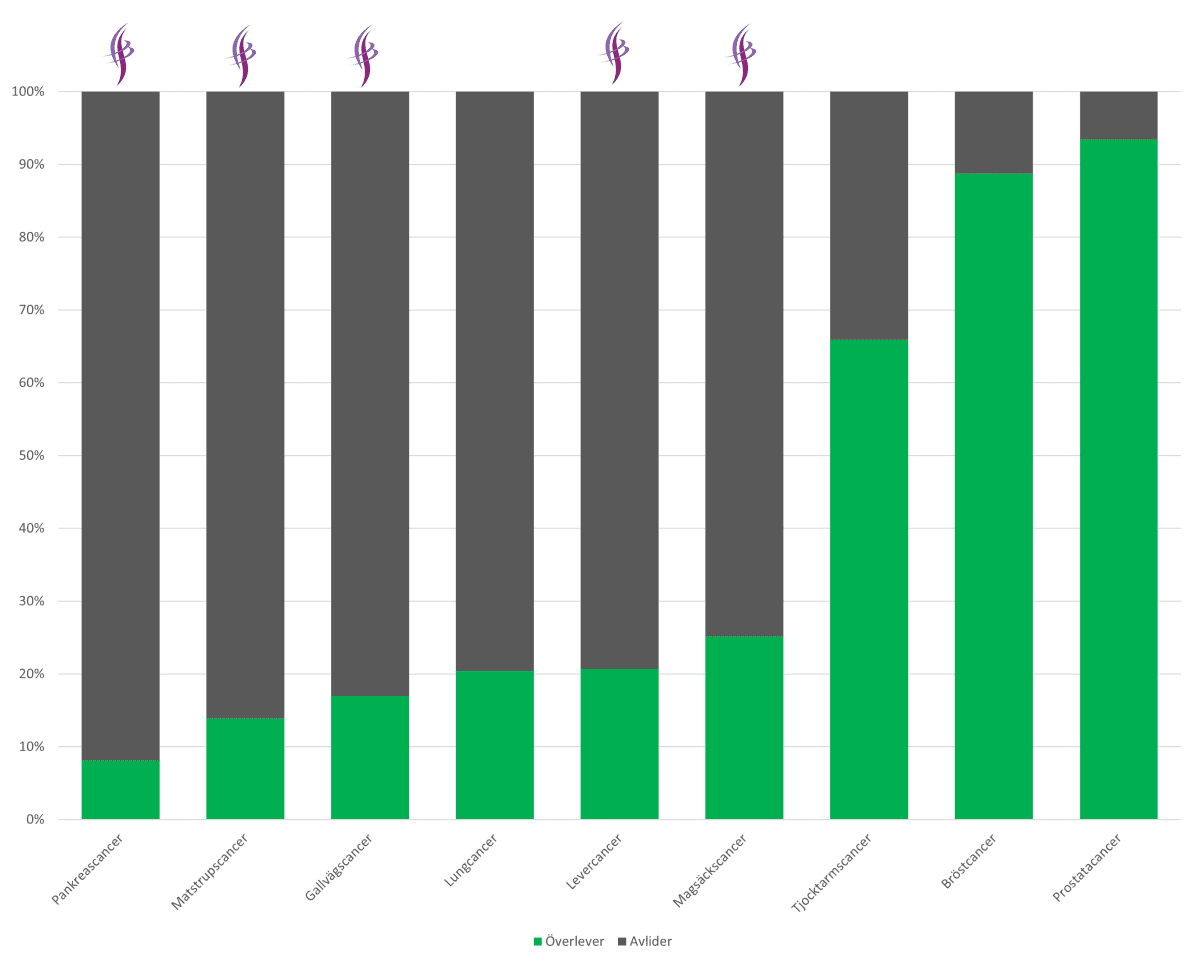
5-year survival rate
Here is the bar chart which is very informative.
For pancreatic cancer
- 1 in 12 (8%) survive 5 years.
- Over the last 50 years, survival rates have only increased from 3 to 8%.
For liver/bile duct cancer
- 1 in 5 (19%) survive 5 years.
- For liver cancer, the 5-year survival rate is 21%.
- For bile duct cancer, it is 17%.
- There has been no significant improvement in survival in liver cancer or bile duct cancer in recent years.
For gastric/esophageal cancer
- 1 in 5 (19%) survive 5 years.
- For gastric cancer, the 5-year survival rate is 25%.
- For esophageal cancer it is 14%.
- In 15 years, survival rates have not changed significantly.
For all types of cancer
- Mortality rates that are much higher than the average.
- Cancer that is detected at a late stage because early and clear symptoms are missing.
- Cancer that is time-critical, meaning it spreads quickly.
- Cancer is what the EU calls “a neglected cancer” when it comes to resources for studies, research and development of new treatments.
All figures come from the National Board of Health and Welfare’s ‘Cancer in Figures’ and are from 2016. See all details here (PDF).
Should only our types of cancer be classified as emergency cancer?
All cancer is serious and usually becomes a fatal disease if not treated. All cancer should be prioritized. However, some rare types of cancer are of an emergency nature and more complicated than others, as shown above.
The types of cancer that we at PALEMA represent are particularly acute as they are usually detected late and spread extremely quickly. Time becomes a critical factor. And these are the ones we want to classify as emergency cancer – an emergency disease that cannot wait!
Unfortunately, over the years we have read in the media about people dying from our types of cancer because they had to wait for treatment. In other countries, for example, pancreatic cancer is an emergency disease that requires rapid action if there is to be a chance of a cure. The current Swedish healthcare system is not able to deliver this, so it is important to establish a classification – an emergency cancer that provides a fast track to investigation and treatment.
For those with other medical problems – such as the elderly who are mostly affected by our types of cancer – further examinations may be needed, often by other specialists, which further delays the process.
In some countries, cancer assessment, additional investigations and treatment planning take place within one day with a plan for surgery within 2-3 weeks.
Prompt treatment is a must
There are big differences in how quickly people are diagnosed and can start treatment. For some types of cancer, drop-in appointments and the opportunity to get an assessment within 2 weeks is offered – while others may have to wait for months. The time from first contact to suspicion to treatment is often far too long for our types of cancer.
Serious side effects
Curative treatment often involves heavy oncological treatment with chemotherapy and/or radiotherapy, sometimes before and sometimes after removal of the tumor. A treatment that often lasts for several months to reduce/stabilize the tumor burden and thus enable curative surgery.
Both oncological and surgical treatments have side effects and complications, which means that rehabilitation time is more often counted in six months and years than in weeks and months.
Patients who make it through these tough treatments often suffer severe, lifelong side effects. Rehabilitation is of utmost importance, but unfortunately there is a lack of clear national guidelines and support.
Read more about each type of cancer here:
What we call for
We share a zero vision of a cancer-free society with everyone – that one day we can say we have eradicated cancer as we have done with polio, tuberculosis and other previously very deadly diseases.
But our types of cancer have a long way to go – we are at the bottom of the statistics in terms of survival. Now we aim to change this by
1. Emergency condition
Our types of cancer should be classified as emergency cancer and therefore treated as emergency conditions.
2. Early detection
Awareness of our types of cancer must be increased in primary care. Several studies show that many people seek primary care several months before they are diagnosed with cancer. Misdiagnosis is common and delays cancer diagnosis.
A national, digital decision support system that identifies symptoms, warning signs and abnormal patterns must be developed and implemented in primary care.
3. National MDK
All difficult cases where our types of cancer are suspected should be referred to and managed by the national MDK (Multi-disciplinary conference) where specialists and the profession discuss treatment options.
4. Multidisciplinary centers
Our types of cancer should be treated in a few certified nationwide specialized centres – “CCCs of excellence”.
5. Certified care
Surgery/treatments for our types of cancer should be performed by experienced and certified doctors and healthcare professionals. A “driving license” based on documented experience, suitability, specialist training etc. for our types of cancer ought to be required.
6. specialist training
To become certified, health care staff ought to have undergone specialist training, been assessed as suitable and assisted in a number of treatments.
7. 24/7 support (around the clock – all week)
There should be a 24-hour emergency number for specialist care in case of complications during treatment. There should also be a direct line of communication after the end of treatment.
8. Quality registers
All variables for our types of cancer should be reported to the quality register.
Our requests
In addition to the above, we also urge the following:
9. Gene sequencing
If one of our difficult types of cancer is suspected, gene sequencing should be carried out at an early stage of the investigation. With so few treatment options, knowledge of the patient’s tumor biology is of utmost importance for potential new treatments, participation in studies, etc.
10. Ongoing responsibilities
Specialised healthcare should be responsible for the patient even after treatment has been completed. Relapses and severe complications are very common and require specialist support. Regular monitoring/screening for early relapse is mandatory.
11. Proactive work
Specialist centers should be proactive towards patients. Patients should not have to “chase” healthcare and become their own project managers. Handovers between departments should always be active.
12. Information on the treating doctor
Patients should have the right to receive information about their doctor’s experience – for example, how many operations and treatments he or she has performed.
13. Freedom of choice
Patients should have the right to choose where they receive their treatment. Readily available, adequate information and statistics should be available on the tiered structure – which hospital(s) are best in terms of safety, volume, quality and patient satisfaction variables.
As a patient, you should also have the right to choose the doctor you want to treat you. Information relating to experience – such as the number of operations and treatments performed – should therefore be readily available.
14. Research and innovation
More research and innovation is needed for our types of cancer.
Share – Email – Print: